Introduction: Sickle Cell Disease (SCD) is a deadly, painful set of genetic abnormalities primarily affecting patients of African and Mediterranean descent.
Although the hallmark symptom of SCD is pain, it is a multi-system disease that results in an amalgam of severe and life-threatening health consequences including increased susceptibility to bacterial, viral, and fungal infections. Infection remains the leading cause of morbidity and mortality in individuals diagnosed with SCD.
We identified no research focused on the treatment patterns of antibiotic utilization in adults with SCD. This dearth of literature specific to SCD is surprising since the first 24 hours of antibiotic treatment in patients with SCD, especially those at risk for recurrent infection could reduce life threatening complications, length of hospital stay, and overall healthcare expenditures. A standardized protocol for treatment of infections in SCD does not exist and the first 24 hours of treatment varies among physicians and institutions. Treatment plans are determined by consensus guidelines, clinical experience and modifying treatment practices that have have shown promise in other diseases. The purpose of this study is to analyze treatment patterns within the first 24 hours of hospitalization in patients with SCD and infection to identify major factors influencing outcomes and clinical management.
Methods:
We conducted a retrospective cohort study using electronic health records from hospitalizations with a documented infection in North-Central Florida. Encounters from patients with sickle cell disease (SCD) were identified using ICD codes (ICD-9 codes: 282.41, 282.42, 282.61, 282.62, 282.63, 282.64, 282.68, 282.69). Demographics, comorbid conditions, empiric antibiotic use, causative infectious organism, and the presenting infectious syndrome were extracted from EHR for each hospitalization. Outcomes of interest were length of hospitalization and 90-day all-cause mortality. Patients with no listed comorbid conditions at the time of hospital admission were excluded. Patient characteristics and clinical factors between groups were summarized descriptively and compared between SCD encounters.
Results:
Among approximately 140,000 eligible encounters, 988 (0.71%) encounters were from those with SCD and of those 837 were included in the analysis:
Median Age: 47 y/o
Sex: Female 583 (69.7%) Male: 254 (30.3%)
209 (0.25%) had an infection fromE. coli and (12.4%) had an infection from staphylococcus aureus.
332 (39.7%) of hospital admissions were secondary to genitourinary infections
Vancomycin (28.7) was the most frequently used antibiotic within the first 24 hours of admission
More than half (67.4%) of patients had chronic pulmonary disease
The median length of stay during our study period was 7 days
12.1% of encounters required intensive care unit hospitalization
90 Day All-Cause Mortality was 5.5%
Results:
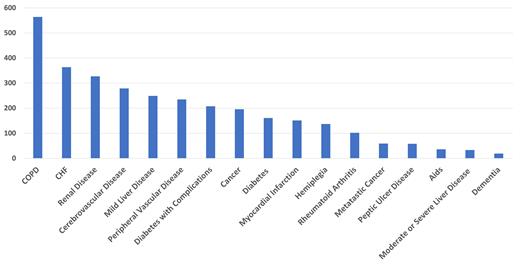
We examined the key comorbid conditions and factors that influence the hospitalization and their outcomes in SCD
Future studies are needed to examine the key factors resulting in an increased risk of infection among SCD genotypes and the treatment patterns within the first 24 hours of treatment in patients with SCD and non-SCD to identify major factors influencing differences in outcomes and clinical management. .
Machine learning approaches could aid in stratifying patients to direct more intensive interventions towards high-risk groups to improve the health outcomes of patients with SCD
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal